Central Vascular Access Device (CVAD)
What is a central vascular access device (CVAD)?
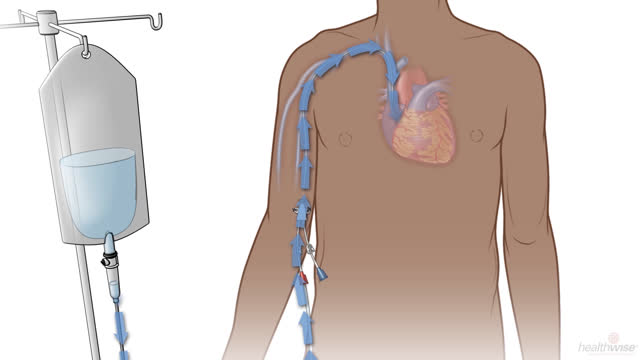
A central vascular access device (CVAD) is a thin, flexible tube. It's also called a central line. It is used when a person needs to receive medicine, fluids, nutrients, or blood products for several weeks or longer. It's often placed in the neck, chest, or arm.
Why is it used?
CVADs are used to:
- Give long-term medicine treatment for pain, infection, or cancer or to give nutrients or blood products.
- Give medicines that affect the heart, especially in an emergency.
- Give large amounts of blood or fluid quickly.
- Receive kidney dialysis if you have kidney failure.
A CVAD may also be used to draw blood for tests.
It may also be used to check blood flow in the heart and body.
What are the types of central vascular access devices?
There are several types of CVADs.
- PICC line. A peripherally inserted central catheter, or PICC line (say "pick"), is a CVAD inserted into a vein in the arm. The part of the line that stays outside the skin may have two or three ends, called lumens, so that you can get more than one medicine or fluid at a time. The end of each lumen is covered with a cap.
- Tunneled catheter. This type of catheter goes into a vein in the neck or chest and is passed under the skin. Medicines and fluids can be given through the end of the catheter that stays outside the skin. Passing the catheter under the skin helps keep it in place better, lets you move around easier, and makes it less visible.
- Implanted port. This type of CVAD is left entirely under the skin. Medicines and fluids are given through the port. Some implanted ports contain a small reservoir that can be filled with medicine that is slowly released into the blood. An implanted port requires very little daily care and may not affect a person's activities.
What are the risks?
Possible problems with a CVAD include:
- Bleeding. This may happen when the device is inserted into a vein. It's usually mild and will stop by itself.
- Pain. You may feel pain where it is inserted or where it lies under your skin.
- Infection. If infection occurs, you will need antibiotics or the CVAD will be removed.
- Blockage. Regular flushing of the CVAD helps reduce blockage.
- Kinking. A twisted or kinked CVAD must be repositioned or replaced.
- Blood clots, which can form in veins, especially in the arms.
- Shifting. If the CVAD has moved out of place, it can sometimes be repositioned. If this doesn't work, it must be replaced.
- Rarely, a collapsed lung (pneumothorax). This would occur during placement of the CVAD.
How can you care for a central vascular access device at home?
You can take the following steps at home to care for your CVAD.
- Always wash your hands with soap and water before touching your device.
- Try to keep the device dry. This can help prevent infection. When you shower, cover the device with waterproof material, such as plastic wrap.
- Fasten or tape the device to your body. This can prevent it from being pulled on.
- If your device has a clamp, keep it clamped when you are not using it.
- Do not wear clothing that rubs or pulls on the device.
- Don't wear jewelry, such as necklaces, that can catch on the device.
- Talk to your doctor about what activities you can do.
- Avoid bending or crimping your device.
- Clamp off the device if it breaks. Then go see a doctor as soon as possible.
- Your device will need regular flushing to keep it open. Your care team may do this for you. You or a caregiver can be taught to do this at home.
- Carry a medical alert card with you, and consider wearing a medical alert bracelet. These will tell health care providers you have a CVAD in case you need emergency care.
When should you call for help?
Call 911 anytime you think you may need emergency care. For example, call if:
- You passed out (lost consciousness).
- You have severe trouble breathing.
- You have sudden chest pain and shortness of breath, or you cough up blood.
- You have a fast or uneven pulse.
Contact your doctor now or seek immediate medical care if:
- You have swelling in your face, chest, neck, or arm on the side where the line is.
- You have signs of a blood clot, such as bulging veins in your neck.
- You have fluid leaking from around the line.
- You feel resistance when you inject medicine or fluids into your line.
- Your central line is out of place. This may happen after severe coughing or vomiting, or if something pulls on the line.
- You have symptoms of infection, such as:
- Increased pain, swelling, warmth, or redness.
- Red streaks leading from the line.
- Pus or blood draining from the line.
- A fever.
Watch closely for any changes in your health, and be sure to contact your doctor if you have any problems.
Related Information
Credits
Current as of: October 1, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 1, 2025
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Ignite Healthwise, LLC education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.